References:
1. Guo Y, Tian X, Wang X, Xiao Z. Adverse effects of immunoglobulin therapy. Front Immunol. 2018(9)1299:1-13.
2. Hooper J. The history and evolution of immunoglobulin products and their clinical indications. J LymphoSign. 2015;2(4):181-194.
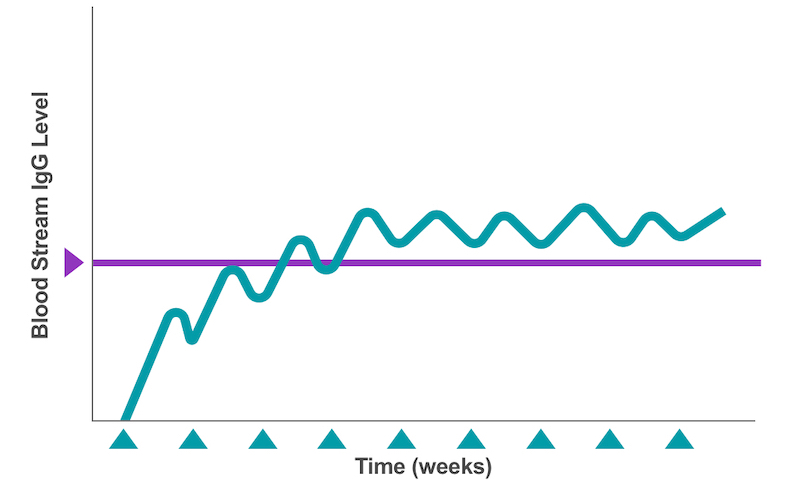
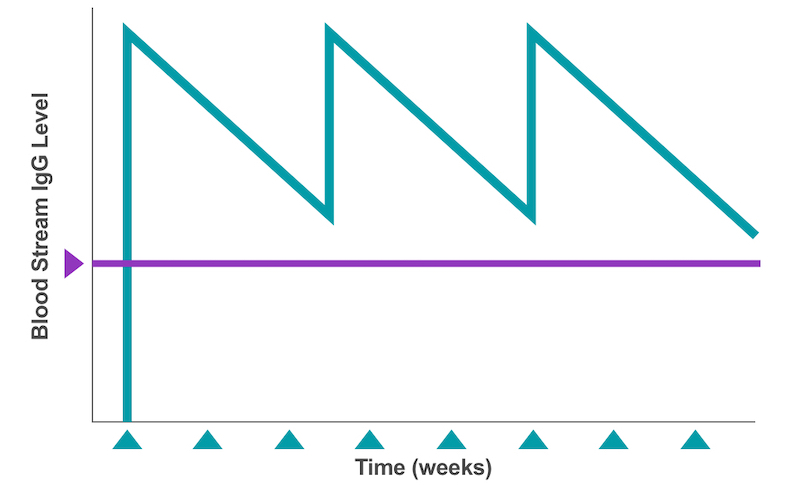
3. Kobrynski L. Subcutaneous immunoglobulin therapy: a new option for patients with primary immunodeficiency diseases. Biologics. 2012;6:277-287.
4. Chapel H, Prevot J, Gaspar HB, et al. Primary immune deficiencies – principles of care. Front Immunol. 2014;5(627):1-12.
5. Ness S. Differentiating characteristics and evaluating intravenous and subcutaneous immunoglobulin. Am J Care. 2019;25:S98-S104.
6. Berger, M. Choices in IgG replacement therapy for primary immune deficiency diseases subcutaneous IgG vs. intravenous IgG and selecting an optimal dose. Current Opinion in Allergy and Clinical Immunology. 2011;11(6),532–538-532.
7. Levasseur, M, Haddad, É. Improved quality of life with home therapy with subcutaneous immunoglobulins for patients with secondary hypogammaglobulinaemia. Allergy, Asthma, and Clinical Immunology : Official Journal of the Canadian Society of Allergy and Clinical Immunology. 2012;8(Suppl 1):A26.
8. Gelbmann, N, Zöchling, A, Pichotta, A, et al. Octanorm [cutaquig®], a new immunoglobulin (human) subcutaneous 16.5% solution for injection (165 mg/mL) – Biochemical characterization, pathogen safety, and stability. Biologicals. 2019;(60):60-67.
9. Skoda-Smith, Torgerson, Ochs. Subcutaneous immunoglobulin replacement therapy in the treatment of patients with primary immunodeficiency disease. Ther Clin Risk Manag. 2010;6:1-10.
10. Bonilla FA. Intravenous immunoglobulin: adverse reactions and management. J Allergy Clin Immunol. 2008;122:1238-1239.
11. Espanol T, Prevot J, Drabbwell J, et al. Improving current immunoglobulin therapy for patients with primary immunodeficiency: quality of life and views on treatment. Patient Prefer Adherence. 2014;8:621-629.
12. Perez EE, Orange JS, Bonilla F, et al. Update on the use of immunoglobulin in human disease: A review of evidence. J Allergy Clin Immunol. 2017;139(3):S1-S46.
13. Stiehm ER. Adverse effects of human immunoglobulin therapy. Transfus Med Rev. 2013;27(3):171-178.
14. Immune Deficiency Foundation. IDF Guide to IG Therapy. Epland K, Perez EE. Townson, MD: Immune Deficiency Foundation; 2018.
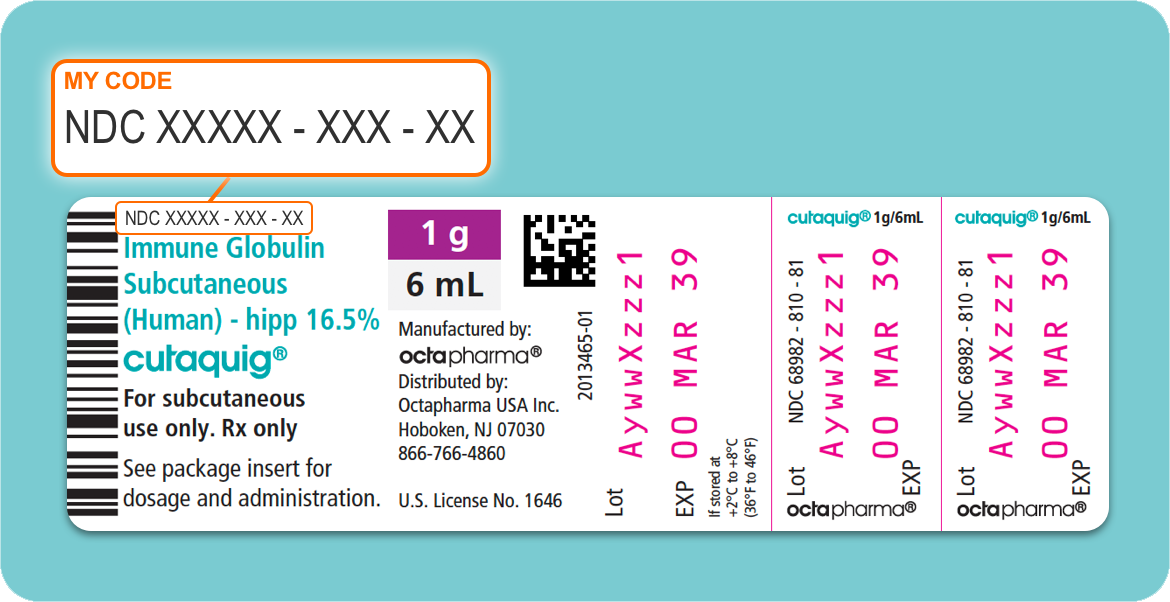
15. Cutaquig Full Prescribing Information. Paramus, NJ: Octapharma; rev October 2021.
16. Wasserman RL. Common infusion-related reactions to subcutaneous immunoglobulin therapy: managing patient expectations. Patient Prefer Adherence. 2008(2):163-166.
17. Zuizewind CA, van Kessel P, Kramer CM, et al. Home-based treatment with immunoglobulins: an evaluation from the perspective of patients and healthcare professionals. J Clin Immunol. 2017;38:876-885.