Lifestyle and Quality of Life Considerations
The following are decision points you should consider and discuss with your healthcare provider when evaluating which route of administration is right for you.
Site of Care
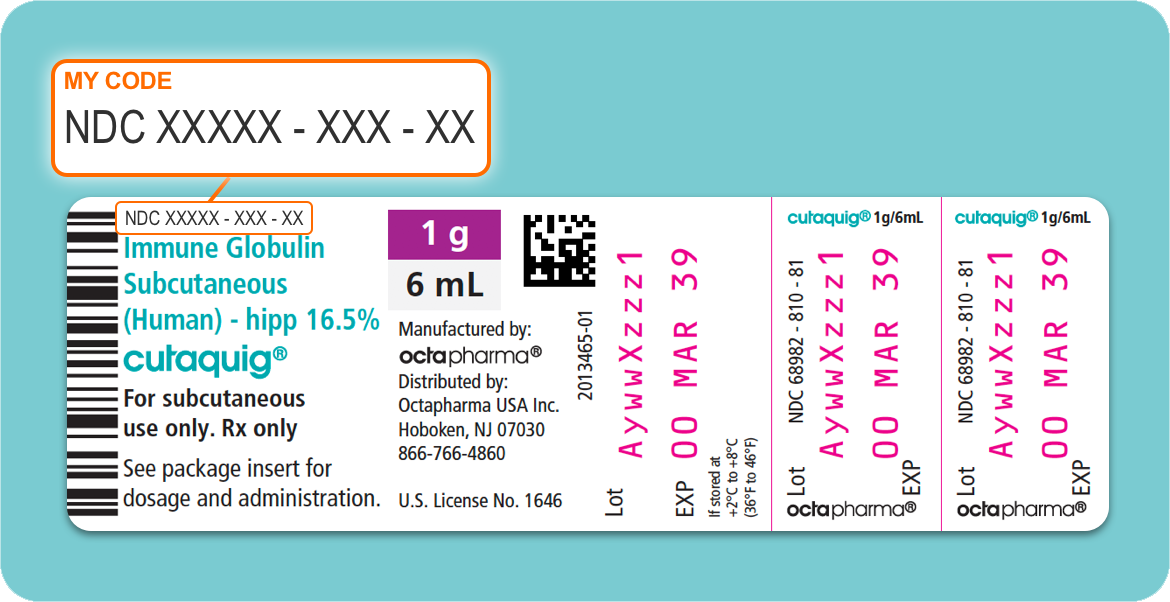
Which form of Ig administration a patient prefers is an important factor that healthcare providers often consider when choosing between IVIg and SCIg.2 However, the options available for where a patient would prefer to receive their infusions (called the site of care) are also an essential factor when choosing the right product.2 Some options for site of care include:2
- Hospital inpatient facilities with healthcare provider supervision
- Hospital outpatient facilities with healthcare provider supervision
- Doctors office with healthcare provider supervision
- Infusion suite with healthcare provider supervision
- Home-based infusion with healthcare provider supervision
- Home-based infusion without healthcare provider supervision
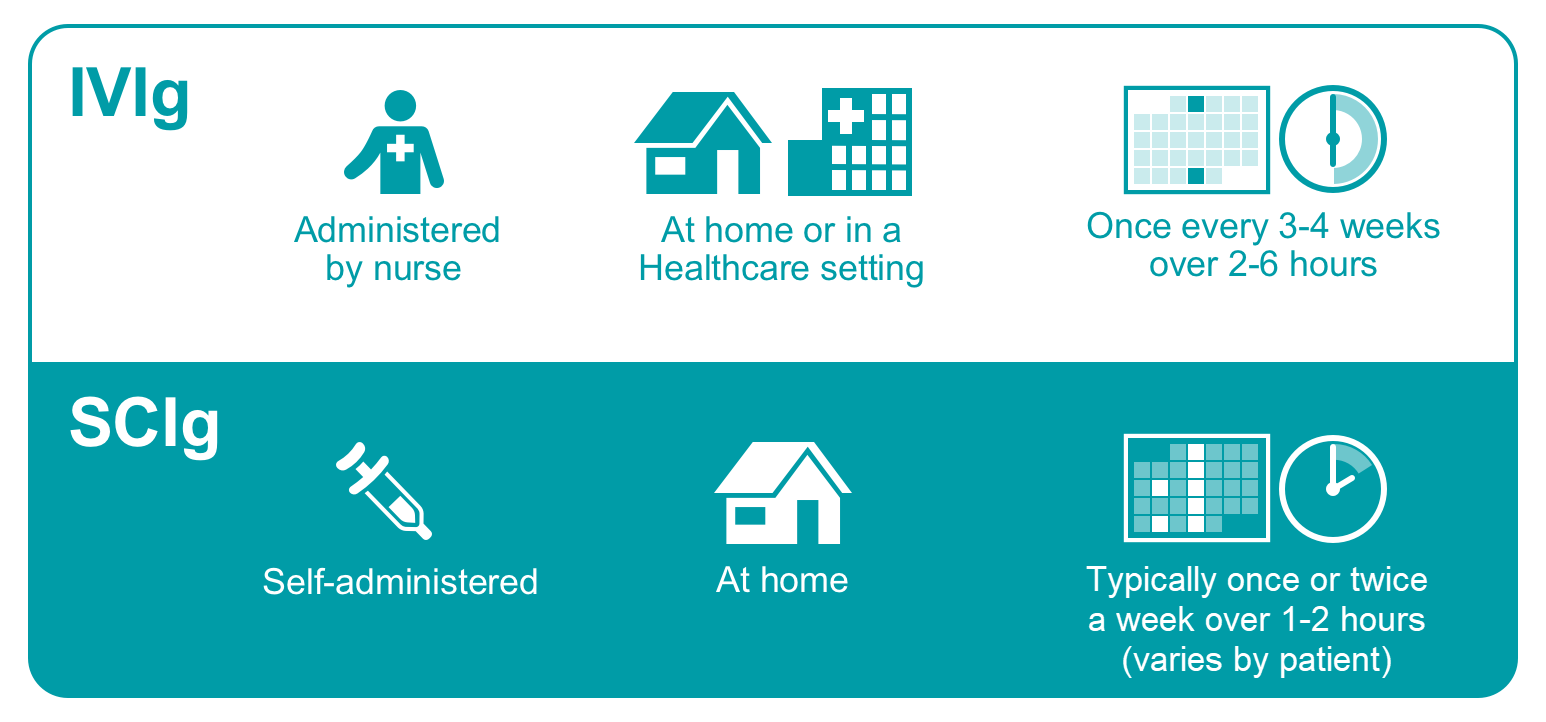
Although home-based treatment is an option for both IVIg and SCIg therapies, only SCIg offers the benefit of self-administration, which eliminates the need for a nurse’s supervision.2 Data from patient surveys show that many patients prefer the convenience and independence associated with the at-home, self-infusion options offered with SCIg.9
Being able to self-infuse at home is a unique benefit of SCIg; however, prescribers usually consider a range of factors before determining which site of care and route of administration is best for the patient. These specifics can include:2
- The patient’s medical history and pre-existing diseases
- Age
- Ability to travel
- Home environment
- Previous experiences with IgRT
- Access to emergency services
- Availability of a caregiver
- Third-party payer restrictions
- Financial burden
- Patient preference
The choice of which product to administer and where to administer it often depends on a joint decision-making process, where the prescriber’s judgement and patient’s preferences, medical, or individual needs, and sometimes insurance coverage, are all taken into account.8
Doses and Frequency
Because with IVIg the full monthly dose of immunoglobulin is administered all at once directly into the patient’s bloodstream, it can often lead to a rapid and high rise in IgG concentration levels (called a peak), followed by a rapid fall over the next few days (called a trough).2,9 These peaks and troughs can be associated with mild to moderate unwanted side effects, called adverse events, and a drop in energy (fatigue) as the IVIg “wears off.”9,11 This “wear-off” is often a reason why some patients prefer SCIg over IVIg.11
Conversely, SCIg regimens that are given under the skin are associated with smaller and more frequent doses. This alternative dosing schedule can reduce the risks of the systemic adverse events (meaning harmful side effects that occur inside the body) typically associated with IVIg.9 The smaller doses and more regular intervals of SCIg can result in higher and more stable IgG trough levels than with IVIg, helping to avoid “wear off”.9 The downside to these regimens, however, is that the underlying skin tissue cannot accommodate large volumes of SCIg fluid.9 This requires that patients infuse smaller volumes, more often, and at more injection sites than is needed with IVIg administration.9 The amount of needle sticks and number of injection sites typically required to administer a full dose of SCIg can often lead to local adverse reactions (unwanted side effects that happen at the site of the injection).9
Route of Administration
During an IVIg treatment session, a nurse who is trained in the administration of IVIg will use a single needle (called a catheter) to infuse the full monthly dose of prepared Ig formulation all at once directly into a patient’s vein.10
During an SCIg infusion, a patient or patient’s caregiver will use a needle set explicitly designed for SC infusions to inject the prepared dose under the skin.2,7 Depending on the patient’s individual tolerance to the therapy, these infusions can be given daily, weekly, biweekly, or every 3 to 4 weeks until the full monthly dose is infused.2,4,7 Multiple SC sites can be injected simultaneously into the skin on the belly, inner thighs, outer buttocks, upper arms, or lower back.7 Where to stick the needles and how many needles sticks will be required, depend on how much SCIg is going to be infused that day. Sometimes, only one injection site is required; other times, many sites are needed at once.7
Not all routes of administration are appropriate for all patients. For example, patients who may have difficulty accessing a vein may not be viable candidates for IVIg.2 Patients who do not have cognitive or fine motor abilities, or who may have a fear of needles, may not be able to self-infuse, so SCIg may not be the right option for them.2,8
Although each route of administration has unique qualities that may be advantages or disadvantages and may not be appropriate for every patient, the ultimate decision remains a patient-specific choice.2
Adverse Reactions
Determining which method of IgRT administration is best for any given patient requires an assessment not only of the benefits of the therapy and preferences of the patient, but also of the risks. While the typical long-term safety of Ig preparations has been well established, and both IVIg and SCIg are well-tolerated and considered safe for most patients, adverse events can occur.2,5,7,12
Adverse events in patients undergoing IVIg therapy tend to be systemic (throughout the body) and are observed more often in patients who are new to IgRT.2 The most common systemic reaction reported in the literature is mild or moderate headache, which can occur either during or after an infusion.7,9,14 Other reactions can also include fatigue, fever, chills, or “flu-like” symptoms.14 On the other hand, systemic adverse events are rare with SCIg and most adverse reactions tend to be mild local site reactions that decrease over time, including localized swelling, redness, itching, and soreness.2,7,9,12,13
Check out our article comparing side effects of SCIg and IVIg routes of administration for additional details.
Quality of Life Impacts
IgRT is the most widely encountered treatment option for patients with PI. There is good evidence that the therapy prolongs survival and reduces morbidity (or sickness).2,9 Both IVIg and SCIg have been shown to protect patients from serious bacterial infections and improve their health-related QoL.8,9
That said, several studies indicate that many patients prefer the autonomy and perceived health benefits associated with SCIg therapy.7 They reference preferences for:
- Improved sense of well-being7
- Increased health-related function and improved self-rated health13
- Higher patient and family sense of independence and self-mastery13
- Flexibility of regimen and self-administration at home11,13
- Ease of administration7
- Speed of administration9
- Convenience of administration; fitting into patient schedules7,9,11
- Better treatment tolerance and fewer systemic reactions11
However, SCIg is not for everyone. Those who prefer IVIg therapy cite dissatisfaction with several aspects of SCIg treatment:
- Number of needles required per month9
- Frequency of infusion9
- Perceived inconvenience11
- Concerns about adverse reactions at home11
- Fear of frequent needle sticks11